Click here to register!
Electrification of Six Health Centres in Rhino Camp and Imvepi Refugee Settlements
Background
Uganda is one of the twenty countries with the largest population that lacks access to electricity, with only 43% of the population having access. The importance of reliable, sustainable and accessible energy for health centres is undebatable. Based on the results from the 2007 Uganda Service Provision, 58% of health facilities did not have access to electricity and only 15% had “reliable” electricity. When further disaggregated by type of health facility, 60 % of lower-level health facilities lack access. Given this background, the GIZ projects Energy Solutions for Displacement Settings (ESDS) and Energising Development (EnDev) intended to provide and install OGS PVS for 6 purposefully selected health centres located within Rhino Camp and Imvepi Refugee Settlements in Terego and Madi Okollo districts of Uganda in 2021. This article provides a summary of the baseline assessment results that was conducted in 2021 prior to the electrification of these six health centers.
Baseline Assessment Results
Five health facilities fall under the direct managing authority of the Ministry of Health (MOH) and one health facility is under the direct managing authority of International Rescue Committee (IRC). Regardless of managing authority, all health facilities receive support – technical, infrastructural, staffing, and other – from the Ministry of Health, a multitude of implementing partners, and UNHCR. The managing authority of health facilities have important implications on the engagement of stakeholders for ownership, maintenance, and sustainability of the OGS PVS assets.
General health facility characteristics (data collected from 2021 Baseline Health Facility Survey).
| Health Center | Refugee Settlement | District | Health Facility Level | Managing Authority | Years of Service | Catchment Population | ||
| Refugee | Host | Total | ||||||
| Imvepi HC II | Imvepi | Terego | HC II | MOH | 26 | 19,668 | 3,224 | 22,892 |
| Yinga HC III | Imvepi | Terego | HC III | MOH | 25 | 10,813 | 7.351 | 18,164 |
| Siripi HC III | Rhino Camp | Terego | HC III | MOH | 27 | 13,090 | 5,500 | 18,590 |
| Ofua HC III | Rhino Camp | Terego | HC III | IRC | 5 | 26,952 | Unknown | Unknown |
| Ocea HC II | Rhino Camp | Madi Okollo | HC II | MOH | 26 | 18,428 | 3,729 | 22,157 |
| Odoubu HC II | Rhino Camp | Madi Okollo | HC II | MOH | 29 | 12,461 | 4,500 | 16,961 |
Status of Electrification
None of the six health centres were connected to the national or community grid. However, all six health centres had at least one partially function OGS PVS and 3 health facilities had at least one diesel generator. Five had standalone EPI solar refrigerators to store and ensure cold chain of vaccines and oxytocin. Four had a We Care Solar installed to charge small devices, such as the HemoCue, Foetal Doppler, and mobile phone, and only 3 of the We Care Solar are functional as the battery of the We Care Solar was stolen at one facility. Finally, Two health facilities had Mobile Power (MoPo) power banks to provide additional power.
Electricity and Health Service Delivery at the Health Centers
According to the five facility in-charges under MOH, the first solar panels were installed when the health facilities were established for the arrival of the first wave of refugees from South Sudan over 20 years ago. Multiple partners, including Care International, Danish Refugee Council, and UNICEF, have since donated and installed different OGS PVS in select wards/ departments/ units and staff quarters.
While each health facility appears to have many OGS PVS, few of them are fully functional. Healthcare workers report frequent interruptions of electricity at the health facility and have developed multiple strategies to mitigate the impact of energy deficit on health service delivery. These mitigation strategies are categorized into four main categories: conserving energy for emergency use, finding alternative systems for energy, use of manual, non-electric methods in consultation, diagnostic, sterilization of equipment, and reporting, improvising locale of service delivery to access energy (e.g., moving patient to another ward to access lighting or electricity) and patient referral to another health facility or sending out patient samples for analysis at another laboratory.
Maintenance of the energy systems
For diesel systems, all 3 health facilities reported having a routine preventive maintenance program. However, they do no have their own strategies for repair and replacement but rather report to donor in such cases. Only one facility had trained staff on maintenance and one reported on having an O&M manual.
For solar systems, 3/6 reported having a routine preventive maintenance programme for their solar systems. 1/6 reported receiving maintenance support from an external technician 2/6 reported performing on-site cleaning of the solar arrays, but without a specialized technician. If there were problems with the solar systems at the health facility, 2/6 facilities said they would call the donor for replacement and 4/6 facilities said they did not have a formalized system in place. None of the facilities reported having staff trained on how to maintain a solar system and one health facility (1/6) reported having an O&M manual for the solar system.
Ownership of Solar Systems
There is limited sense of ownership for the existing OGS PVS with the exception of the Mobile Power charging stations. In case of any failure, the health facility’s strategy is to call the district or the partner for help and replacement. According to several healthcare workers, capacitating the staff to look after the solar systems can help them feel ownership and responsibility towards these assets.
Capacity building for maintenance of the solar systems
None of the health centres are capacitated to provide routine maintenance of the solar systems and od not have designated staffs for O&M of the existing OGS PVS. In general, interviewed healthcare workers and HUMC members showed wiliness to learn basic O&M skills. The District Health Officer noted that Arua Regional Referral Hospital’s equipment maintenance unit has existing capacity and expertise which could be leveraged on.
Funding for maintenance, repair, and replacement of solar systems
The primary source of funding is donors grants and apart from that two additional sources like Capital Development Fund and the District Development Equalization grant were identified. For health facilities manged by MOH, the funding sources include: Primary Health Care (PHC) Fund and Results-Based Financing.
As a result of limited funding opportunities and the recognition that repairs and replacements of solar components, such as batteries will exceed what is available from the PHC funds, HUMC, health facility staff, and district health officers feel that GIZ should budget funds to support the maintenance of OGS PVS. HUMC and healthcare workers are eager for support to initiate income-generating activities in order to generate funds to support the minor maintenance and repair of the solar systems. Each site had its own ideas of what would work in its setting (see below table). Notably, these income-generating activities would need an injection of start-up capital in order to be functionalized.
Recommendations
1. Ensure adequate sizing of solar systems to fully functionalize health service delivery
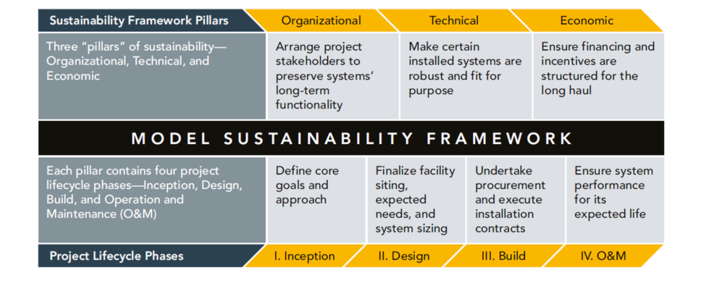
2. Develop and implement an O&M plan for each health facility
3. Develop and implement a sustainability plan for each health facility
4. Leverage health system strengthening opportunities with the anticipated improvement in availability and reliability of electricity
5. Measuring impact