Difference between revisions of "Energy for Rural Health Centers"
***** (***** | *****) |
***** (***** | *****) m |
||
| (193 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
| − | |||
| − | |||
| − | |||
| − | = | + | == Introduction == |
| − | = | + | [[File:Image RIIP.jpg|700px|alt=Image RIIP.jpg|right]] |
| − | + | Health professionals in rural clinics face many challenges on a daily basis. Not only a lack of qualified medical staff, equipment and medicine can become a major obstacle in providing crucial basic health services for the rural population, also lacking or unreliable energy supply can be a severe problem. | |
| − | + | If the cold chain is inoperable when supplies arrive, vaccines, blood, and other medicines may go to waste. Without proper electric lighting, most medical treatments can only be conducted at daytime, while emergency surgeries at night may only be illuminated by dim kerosene lamps or torches. Also for the provision of water, energy is frequently required for pumping and heating. | |
| − | + | <br/> | |
| − | + | Despite its high relevance for the provision of health services, there is little reliable data on energy access in health facilities in developing countries.<br/> | |
| − | + | <br/> | |
| − | + | In India, Rural Health Statistics 2018 data showed nearly 22% or 40,000 primary health centers in rural India are still operating without electricity supply.<ref>India Today (2019). https://www.indiatoday.in/india/story/after-4-years-of-swachh-bharat-38-percent-govt-health-centres-in-rural-india-without-staff-toilets-1623694-2019-12-04 </ref><br/> | |
| − | = References = | + | A review led by the World Health Organization (WHO) in 2013 found nationally representative data for only 14 developing countries globally, 11 of them in sub-Saharan Africa. According to this review, one in four health facilities in Sub-Saharan Africa had no access to electricity, while only 28% of health facilities and 34% of hospitals had reliable access to electricity.<ref name=":0">WHO, The World Bank (2015): [https://apps.who.int/iris/bitstream/handle/10665/156847/9789241507646_eng.pdf%3Bjsessionid=05BA6EDD62617D7CFB7AE8FBE47A639A? Access to modern energy services for health facilities in resource-constrained settings: a review of status, significance, challenges and measurement.]</ref> |
| + | |||
| + | A recent survey of 78 countries found that only 41% of low- and middle-income country health care facilities have reliable electricity.<ref>UN Foundation, SEforALL (2019): Lasting impact – Sustainable off-grid solar delivery models to power health and education. https://poweringhc.org/wp-content/uploads/2019/04/Lasting-Impact_Sustainable-Off-Grid-Solar-Delivery-Models-to-Power-Health-and-Education.pdf</ref><br/> | ||
| + | |||
| + | This is not only hampering proper medical services, electricity outages also can damage medical and diagnostic devices. | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | In addition to electricity, health facilities need thermal energy for cooking, heating, and sterilization. This demand is mostly met by direct combustion of fuels like kerosene, diesel, biomass or gas.<br/> | ||
| + | |||
| + | The widespread use of fossil fuels like kerosene for lighting or diesel for power generation, as well as biomass in inefficient cookstoves cause additional risks to staff, patients and the environment due to emission of particulate matter, black carbon and CO2, and fire hazards.<ref name=":0" /> | ||
| + | |||
| + | Selecting appropriate sources of reliable and sustainable energy as well as introducing measures for efficient energy consumption can help mitigate some of the challenges inherent in operating a health facility in the developing world. | ||
| + | |||
| + | This article will provide an overview on options for the improvement of the energy situation in rural health facilities. | ||
| + | |||
| + | |||
| + | == Electricity in Healthcare Facilities == | ||
| + | |||
| + | Health facilities have different energy needs according to their services provided and on consequently required loads. Some of the basic services include vaccine refrigeration, light, medical equipment, and surgical treatment. Further services include e.g. communication, water pumping and heating, space heating or cooling. | ||
| + | |||
| + | Successful development of reliable energy systems requires careful assessment of all aspects of health facility energy needs, including both electric and thermal energy needs. | ||
| + | |||
| + | Growing energy needs and foreseeable load increases in the near future also need to be considered when analyzing and determining a facility’s load profile. Procurement of more or less energy-efficient medical equipment will influence the future load profile, as will energy-saving retrofits to the building itself. For more information about building efficiency, see WHO/World Bank 2015.<ref name=":0" /> | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | === Classification of Health Facilities === | ||
| + | |||
| + | Healthcare posts and clinics can be distinguished into three categories, namely low, medium, and large health facilities with different energy requirements accordingly.<ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref><ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref><ref name="Smart Villages (2017): Electrification of health clinics in rural areas: Challenges and opportunities. https://e4sv.org/wp-content/uploads/2017/05/TR12-Electrification-of-health-clinics-in-rural-areas-Challenges-and-opportunities_web.pdf">Smart Villages (2017): Electrification of health clinics in rural areas: Challenges and opportunities. https://e4sv.org/wp-content/uploads/2017/05/TR12-Electrification-of-health-clinics-in-rural-areas-Challenges-and-opportunities_web.pdf</ref><br/> | ||
| + | |||
| + | '''Health posts''' are the smallest, most basic facilities. These locations typically will not have a permanent doctor or nurse on staff. They provide basic treatment for emergency cases, first aid, and where possible, basic immunization services. Due to the limited medical equipment used, the overall energy demand of health posts is relatively low. The energy demands of a health post is similar or less than that of a small health clinic. | ||
| + | |||
| + | '''Health clinics''' are generally larger than health posts and employ one or more full-time nurses. A health clinic offers a wider array of services than a health post and will possess equipment allowing for more sophisticated diagnoses. Rural health clinics generally fall into one of three categories (Categories I, II and III - see table below) based on the type and number of medical devices used in the facility and the frequency with which they are used on a daily basis. Local resources may make specific energy options more or less advantageous in each location. | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | The IEA describes the example of a ‘typical’ electrical load distribution of a small health facility in Cambodia (based on PV provision) as 35% lights, 14% fans, 34% lab equipment and 17% other, with the load curve increasing gradually to a midday peak and then decreasing gradually.<ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref> <br/> | ||
| + | |||
| + | Another example load profile of a medium size health facility shows that the highest energy consumption within day time is by laboratory equipment, while lighting systems and fans consume more during the night. The overall electricity distribution, however, shows that the main consumers are lighting systems and fans (57%), followed by lab equipment (29%) and other equipment (14%).<ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref><br/> | ||
| + | |||
| + | Other types of health facilities that require reliable and sustainable electrification include blood banks, stand-alone laboratories and pharmacies, and anti-retroviral treatment (ARV) clinics. Blood banks, stand-alone labs, and pharmacies will, depending on their size, utilize equipment similar to that found in small or medium sized health clinics and will have similar energy needs. ARV clinics will have significant energy demands similar to those found large-sized health facilities.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref><br/> | ||
| + | |||
| + | <br/><br/> | ||
| + | |||
| + | {| style="height: 87px; width: 100px; width: 100%" cellspacing="1" cellpadding="1" border="1" | ||
| + | |+ <u>'''Health Facility Categories''':<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref><ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref><ref name="Smart Villages (2017): Electrification of health clinics in rural areas: Challenges and opportunities. https://e4sv.org/wp-content/uploads/2017/05/TR12-Electrification-of-health-clinics-in-rural-areas-Challenges-and-opportunities_web.pdf">Smart Villages (2017): Electrification of health clinics in rural areas: Challenges and opportunities. https://e4sv.org/wp-content/uploads/2017/05/TR12-Electrification-of-health-clinics-in-rural-areas-Challenges-and-opportunities_web.pdf</ref></u><br/> | ||
| + | |- | ||
| + | | style="background-color: rgb(204, 204, 204)" | '''Category''' | ||
| + | | style="background-color: rgb(204, 204, 204)" | '''Description''' | ||
| + | |- | ||
| + | | style="background-color: rgb(250, 250, 250)" | | ||
| + | '''Category I'''<br/>'''Small / Health clinics or posts'''<br/> | ||
| + | |||
| + | low energy requirements, 5 - 10 kWh/day | ||
| + | |||
| + | | | ||
| + | *Typically located in a remote setting with limited services and a small staff<br/> | ||
| + | *They mainly cater to primary health, with treatments provided for most common diseases such as malaria and TB, in addition to maternal and child health services and first response to emergencies. | ||
| + | *Approximately 0 - 60 beds | ||
| + | |||
| + | Electric power is required for:<br/> | ||
| + | |||
| + | *Lighting the facility during evening hours and to support limited surgical procedures (e.g. suturing)<br/> | ||
| + | *Maintain the cold chain for vaccines, blood, and other medical supplies - one or two refrigerators may be used<br/> | ||
| + | *Utilizing basic lab equipment - a centrifuge, hematology mixer, microscope, incubator, and hand-powered aspirator<br/> | ||
| + | |||
| + | |- | ||
| + | | style="background-color: #d6e0f5" | | ||
| + | [[Image:BOS Logo grey.png|80px|center|link=https://www.bos-ag.com/?lang=de]] <center><big>'''Sponsored Content'''</big></center> | ||
| + | |||
| + | | style="background-color: #d6e0f5" | | ||
| + | 37 health clinics were electrified with off-grid solar systems, consisting of 800Wp Solar Panels, 2.5kWh Lithium batteries (LiFePO4) and 800VA inverter. Each health clinic has around 20 lights (both indoor and outdoor) and sockets have been provided to power basic lab equipment or for powering laptops if necessary. Each system can provide on an average 3-4kWh of clean energy per day. | ||
| + | [https://www.bos-ag.com/electrifying-health-posts/ Click here for more!] | ||
| + | |||
| + | |- | ||
| + | | style="background-color: rgb(250, 250, 250)" | | ||
| + | '''Category II'''<br/>'''Medium-sized / District health centers'''<br/> | ||
| + | |||
| + | moderate energy requirements, 10 - 20 kWh/day | ||
| + | |||
| + | | | ||
| + | *They cater to larger populations than small rural health posts<br/> | ||
| + | *Approximately 60 - 120 beds<br/> | ||
| + | |||
| + | Electric power is required for:<br/> | ||
| + | |||
| + | *<span>Medical equipment similar to Category I Health Clinic; but frequency of use and number of devices are higher than those of Category I</span><br/> | ||
| + | *<span>Separate refrigerators may be used for food storage and cold chain</span> | ||
| + | *<span>Communication device, such as a radio</span><br/> | ||
| + | *<span></span>More sophisticated diagnostic medical equipment | ||
| + | *Advanced equipment, such as small size X-ray machine. | ||
| + | *Complex surgical procedures, such as dental health surgeries<span></span><br/> | ||
| + | |||
| + | |- | ||
| + | | style="background-color: #d6e0f5" | | ||
| + | [[Image:BOS Logo grey.png|80px|center|link=https://www.bos-ag.com/?lang=de]] <center><big>'''Sponsored Content'''</big></center> | ||
| + | |||
| + | | style="background-color: #d6e0f5" | | ||
| + | Close to 50 health centers have been electrified so far in Malawi. One of the key problems of not having reliable power at health centers is high attrition rates with healthcare staff preferring urban health centers with better facilities. Realizing this problem, we connected staff quarters with the solar off-grid energy system. Each of these systems ranged from 5-20kWp depending on the size and capacity of the health center. This solved two main problems: Basic amenities for the staff and additional revenue from selling excess energy towards maintenance of the systems. These systems are remotely monitored for preventive maintenance, visits are planned every six months, and staff is professionally trained to operate and use the system. | ||
| + | [https://www.bos-ag.com/powering-health-centers-in-malawi/ Click here for more!] | ||
| + | |||
| + | |- | ||
| + | | style="background-color: rgb(250, 250, 250)" | | ||
| + | '''Category III''' '''Large-sized health facility/ District or Regional hospitals''' | ||
| + | |||
| + | high energy requirements, 20 - 30 kWh/day | ||
| + | |||
| + | | | ||
| + | *<span></span>Located in urban off-grid areas or cities | ||
| + | *<span>Approximately 120 beds or more</span> | ||
| + | *<span><span></span></span>Large size facilities function as central hospitals which serve thousands of people. Therefore, their energy consumption is high | ||
| + | *They have several wards and include nursing school, staff house etc. | ||
| + | *May serve as a regional referral center and coordinate communication between several smaller facilities and hospitals in large cities | ||
| + | |||
| + | Electric power is required for:<span><span></span></span> | ||
| + | |||
| + | *Lighting the facility during evening hours | ||
| + | *Staff houses | ||
| + | *Medical equipment and sophisticated diagnostic devices (x-ray machine, CD4 counters, blood typing equipment, etc.) requiring additional power | ||
| + | *Complex surgical procedures | ||
| + | *<span><span>May need to communicate with remote health centers and hospitals by way of telephone, fax, computer, and Internet</span></span> | ||
| + | |||
| + | |- | ||
| + | | style="background-color: #d6e0f5" | | ||
| + | [[Image:BOS Logo grey.png|80px|center|link=https://www.bos-ag.com/?lang=de]] <center><big>'''Sponsored Content'''</big></center> | ||
| + | |||
| + | | style="background-color: #d6e0f5" | | ||
| + | Close to 450kWh lithium batteries and 220kWp PV are installed at 6 rural health units (RHUs) and 2 district hospitals in Mindanao region of Philippines. Reducing the diesel consumption to a minimum (even to zero at some hospitals), cuts fuel expenses and carbon emissions and at the same time provides reliable energy services 24/7. The project is done for International Organisation for Migration (IOM) and financed by the Government of Japan. These hospitals offer range of services, from complex surgeries to diagnostics. Solar systems are powering everything, from sophisticated diagnostic equipment to communications (computers and internet) and also staff quarters. | ||
| + | |} | ||
| + | |||
| + | <br /> | ||
| + | |||
| + | === Electricity Needs === | ||
| + | |||
| + | Some very common and basic devices or services that need electricity are the following: | ||
| + | |||
| + | '''Vaccine refrigeration''' | ||
| + | |||
| + | While refrigerators work 24h/day, they actually do not continuously consume power. To keep the internal temperature constant, the compressor or heater runs in a controlled duty cycle mode. Therefore, in order to obtain information about the daily energy demand of a refrigerator, the device's duty cycle must be determined (e.g. by listening), or by measuring the energy consumption for a period of time.<ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref> | ||
| + | |||
| + | '''Lighting''' | ||
| + | |||
| + | This is a very essential service in rural health facilities, mainly at night. Quality and availability of light significantly improves medical emergency interventions, including first aid, birthing and surgery.<ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref> | ||
| + | |||
| + | '''Medical equipment''' | ||
| + | |||
| + | A microscopes is an essential equipment in rural health facilities. In developing countries, common diseases which include HIV, syphilis, malaria, and anemia are diagnosed using a microscope.<ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref> | ||
| + | |||
| + | '''Sterilization''' | ||
| + | |||
| + | Medical tools, including surgical equipment need to be sterilized. Often, sterilization of equipment by air requires a high temperature up to 160◦C for around two hours, while steam autoclaves, where a temperature of 120◦C is sufficient, are even more effective. Because of the required high temperature, sterilization equipment consumes a considerable amount of energy.<ref name="IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf">IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf</ref> | ||
| + | |||
| + | <br/> | ||
| + | [[File:WAME_newlightfornewlife_imm4ok_Hospital_in_Bahor_Afghanistan_after_electrification.png|alt=WAME newlightfornewlife imm4ok Hospital in Bahor Afghanistan after electrification.png|right|500x500px]] | ||
| + | |||
| + | |||
| + | ==== Basic Needs Assessment ==== | ||
| + | |||
| + | When considering the type of electrification needed to sustain daily operations, a facility must first understand its basic needs. The needs assessment will include an inventory of the types of equipment used in the facility and the power required to operate each device. Understanding the average “daily load”, or the amount of power required to operate equipment under normal working conditions, will influence the choice of power supply. Once the daily energy demand is established, a range of electrification options can be considered. Understanding the need will also provide managers with a realistic budget for procuring, installing, and maintaining the new system. | ||
| + | |||
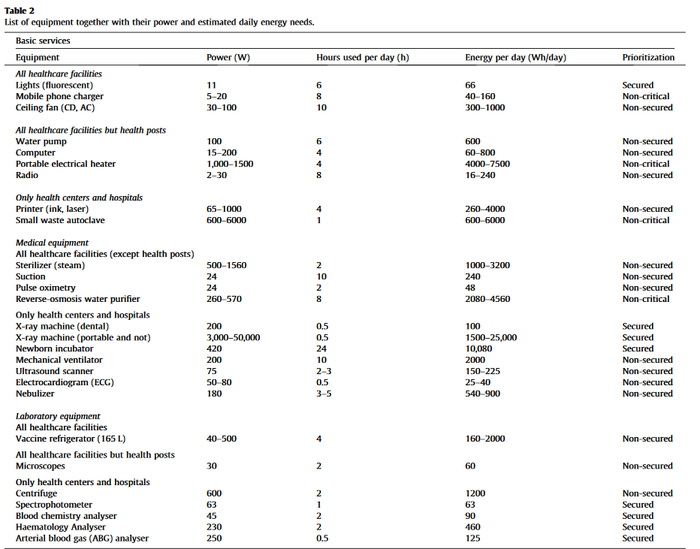
| + | Additionally, when determining how to electrify a healthcare facility, it can also be important to prioritize the electrification of equipment based on its criticality to patients’ survival and the facility’s operation. A. Franco et al. (2017)<ref name="Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub">Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub</ref> propose three categories: non-critical, non-secured and secured. Non-critical refers to equipment that is not critical to patient survival, such as air ventilation in the ward. Non-secured refers to equipment that is critical but can handle moderate voltage fluctuations of the network and short outages, often thanks to an integrated battery. Finally, secured refers to equipment that is critical and needs to be protected against voltage fluctuations. During a power shortage, this prioritization can help in effectively managing electricity production and consumption. | ||
| + | |||
| + | The table below shows a list of common health facility equipment and their respective power needs.<ref name="Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub">Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub</ref> | ||
| + | |||
| + | [[File:Franco et al (2017) Energy Needs of Equipment.png|thumb|center|700px|alt=Franco et al (2017) Energy Needs of Equipment.png]]<br /> | ||
| + | |||
| + | For further information about power requirements of electrical devices for health services see also tables 3 and 4 in the publication “Access to Modern Energy Services for Health Facilities in Resource-Constrained Settings” from WHO / World Bank 2015.<ref name=":0" /><br /> | ||
| + | |||
| + | |||
| + | ==== Tools for Calculating Electricity Needs of a Health Facility ==== | ||
| + | |||
| + | The USAID [http://tools.poweringhealth.org/ Health Clinic Power System Design Tool (4 - Electric Load Inputs)] and/or the [http://www.poweringhealth.org/index.php/resources/tools/energy-audit-spreadsheet Energy Audit Spreadsheet (Worksheet 7 - Future Electric Applications)] as well as the examples of energy demands of typical rural health centers in developing countries can help identifying the overall energy demands of health facilities. The amount of expected energy consumption in kWh/day, in addition to expert consultation, will assists in the selection of appropriate electrification technology. | ||
| + | |||
| + | Once a facility has comprehensively analyzed the energy requirements of its day-to-day operations, likely changes of those demands should be considered. Facility managers must think strategically about the possibility that energy demands may increase due to the addition of patients, extended operating hours, or new services. Once this process has been completed and an adequate accounting of needs has been made, the manager can determine the various energy options to meet those demands. These options must be considered in light of all facility-specific variables. | ||
| + | |||
| + | |||
| + | === Electricity Supply Options === | ||
| + | |||
| + | Once the daily energy demand has been assessed, the next step is evaluating the potential technical solutions for providing sustainable energy services. In areas where access to the national grid electricity infrastructure is available and reliable, this is usually the primary energy source. Wherever this is not the case, off-grid energy systems and on-site power generation solutions must be taken into account. Off-grid energy systems include i.e. generators, renewable energy systems (fueled by solar power, wind power, micro-hydro power), batteries or a combination of two or more of the above-mentioned technologies. The best option for a given application depends on a number of factors, and in some cases a combination of power supply options may be the best solution. | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | <u>Some factors to consider include:<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref></u> | ||
| + | |||
| + | Reliability of local grid<br/>Local renewable energy resources (wind, solar, water)<br/>Local availability of conventional energy sources (diesel, propane, gasoline)<br/>Local capital cost and operating cost<br/>Local availability of systems, parts, service companies, and technicians<br/>Governmental policies and incentives<br/>System reliability requirements<br/>Technical capacity and funds for system maintenance and replacement<br/>Emissions<br/>Special considerations or desired operational characteristics - i.e. noise, etc. | ||
| + | |||
| + | <br/><br /> | ||
| + | |||
| + | ==== Technological Options ==== | ||
| + | |||
| + | *'''Generators''' | ||
| + | |||
| + | Generators run on various fuels, including natural gas, diesel, gasoline and propane. They have been the default onsite power option for a long time, typically powering off-grid facilities. They are also the most widespread back-up energy source for healthcare facilities in the Global South, even for grid-connected facilities.<ref name="Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub">Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub</ref> | ||
| + | |||
| + | The advantage of generators is that they use a consolidated technology with low upfront capital costs. Disadvantages compared to renewables are increasing fuel costs and unstable fuel supply to remote areas (especially in rainy seasons) as well as the role fossil fuels play in global warming. | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | *'''Photovoltaic (PV)''' | ||
| + | |||
| + | Photovoltaic (PV) Systems generate electricity from sunlight collected by solar panels. Energy collected this way can be used to supply direct power to electrical equipment, or it can be stored in batteries to provide indirect power. In combination with a battery, PV systems are excellent for handling small-to-moderately sized loads in locations where grid electricity is not available. They are highly modular, so it is easy to customize the system to the needs of a facility and add units if power demand increases. | ||
| + | |||
| + | As PV converts solar energy to direct-current (DC), photovoltaic systems must be equipped with inverters in order to convert the DC power input to alternating-current (AC) power. Alternatively, devices have to run directly on DC, which is already very common for refrigerators. | ||
| + | |||
| + | In many developing countries harnessing the power of the sun is already widespread for electricity generation. Sharply declining costs, local availability and no emittance of greenhouse-gas emissions makes PV are real alternative to fossil-fueled generators. Standalone solar PV solutions are currently the dominant model for electrifying public institutions, such as health facilities.<ref name="UN Foundation, SEforALL (2019): Lasting impact – Sustainable off-grid solar delivery models to power health and education. http://poweringhc.org/wp-content/uploads/2019/04/Lasting-Impact_Sustainable-Off-Grid-Solar-Delivery-Models-to-Power-Health-and-Education.pdf">UN Foundation, SEforALL (2019): Lasting impact – Sustainable off-grid solar delivery models to power health and education. http://poweringhc.org/wp-content/uploads/2019/04/Lasting-Impact_Sustainable-Off-Grid-Solar-Delivery-Models-to-Power-Health-and-Education.pdf</ref> | ||
| + | |||
| + | Find more info on PV in our [[Portal:Solar|solar portal]] on energypedia. | ||
| + | |||
| + | A very helpful tool, the [https://globalsolaratlas.info/map Global Solar Atlas], with worldwide solar irradiation data per country and region is provided by the World Bank. | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | *'''Wind Energy''' | ||
| + | |||
| + | Depending on the geographical location, wind can be an abundant source of energy. Situating a wind turbine on a site requires careful measurement of wind patterns. Mini and small wind turbines ranging from 1 to 100 kW are mainly used for off-grid rural electrification and can be used in homes and in small communities. Medium and large size wind turbines with capacities ranging from 100 kW to several mega-watts can be used both for on-grid electrification (through connection to the main grid) or off-grid electrification. | ||
| + | |||
| + | Small wind turbines with a diameter of less than 15 m (usually 7 m) require relatively low wind speeds (typically between 3 and 4 meters per seconds, or m/s) for activation, and can thus be employed as an energy source in off-grid healthcare facilities.<ref name="Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub">Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub</ref> | ||
| + | |||
| + | Similar to PV systems, wind turbines must be connected to the grid or to a battery system to provide reliable power. | ||
| + | |||
| + | Find more info on wind energy in our [[Portal:Wind|wind portal]] on energypedia. | ||
| + | |||
| + | A very helpful tool to identify high-wind areas per country and region is the [https://globalwindatlas.info/ Global Wind Atlas]provided by the World Bank. | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | *'''Micro / Pico Hydro''' | ||
| + | |||
| + | In water-rich off-grid settings, micro- and pico-hydropower could also be used for the electrification of healthcare facilities. Micro-hydropower refers to power capacity from 5 kW up to 100 kW, and pico-hydro (up to 5 kW).<ref name="https://en.wikipedia.org/wiki/Micro_hydro">https://en.wikipedia.org/wiki/Micro_hydro</ref> This renewable, clean energy is not intermittent, like solar and wind, though comparable in terms of investment costs. It is the preferred choice for water-rich regions in countries such as Ethiopia, Uganda, Rwanda and the Democratic Republic of Congo.<ref name="Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub">Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub</ref> | ||
| + | |||
| + | Find more info on micro and pico hydro energy in our [[Portal:Hydro|hydro portal]] on energypedia. | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | *'''Hybrid Systems''' | ||
| + | |||
| + | Hybrid-energy systems can include a generator, a PV and/or wind installation and/or hydropower and batteries. This way, limitations of each power system can be overcome and benefits maximized. | ||
| + | |||
| + | With reliable solar and wind resources, a hybrid system will rarely need to rely on a generator. However, it can serve as a backup in case of bad weather. Since the generator can recharge the batteries during prolonged periods of inclement weather, the battery bank in a hybrid system can be significantly smaller than in a PV-battery system, perhaps storing only one or two days’ worth of energy. The low duty cycle minimizes operation costs and extends generator lifetime.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref><ref name="Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub">Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub</ref> | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | *'''Mini-grids''' | ||
| + | |||
| + | <br/> | ||
| + | |||
| + | *'''Grid Extension''' | ||
| + | |||
| + | Grid extension connects the health facility to the local utility. Cost depend on the utility, the terrain, the distance to be covered, and the size of the load to be served. If the local grid is fairly reliable and within a few miles, obtaining an estimate for the capital cost of grid extension and the recurring cost of electricity will give points of comparison when considering other options. | ||
| + | |||
| + | Grid extension typically has a high capital cost, but offers several advantages. First, in most cases, the cost varies only slightly with the size of the load to be served. This makes it uneconomical for small loads but a better option for large loads. Second, once the grid has been extended to the clinic, it can serve other local loads. Third, operations and maintenance are the responsibility of the utility.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> | ||
| + | |||
| + | <br /> | ||
| + | |||
| + | ==== Electricity Technology Characteristics ==== | ||
| + | |||
| + | The table below from USAID (no date, probably published between 2006 and 2010) illustrates the key characteristics of some energy generation technologies. Please keep in mind that costs of renewable energy systems have decreased significantly over the last years, so the assessment provided in the table might have changed. It is also highly dependent on local circumstances, for example import taxes or domestic production, and international fuel prices.<br/> | ||
| + | |||
| + | {| style="height: 315px; width: 100px; width: 100%" cellspacing="1" cellpadding="1" border="1" | ||
| + | |+ <u>'''Energy Technology Characteristics''':<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref></u> | ||
| + | |- | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | Energy Technologies | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | Capital Cost | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | O&M Cost | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | Reliability | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | Durability | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | Special Considerations | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | Emissions | ||
| + | ! style="background-color: rgb(204, 204, 204); text-align: left" scope="col" | Optimal Use | ||
| + | |- | ||
| + | | '''Solar PV System with Batteries''' | ||
| + | | Very high | ||
| + | | Low | ||
| + | | High (if maintained properly) or low (if not) | ||
| + | | 20-30 years (PV), 5 years (batteries) | ||
| + | | Theft (batteries or panels); Vandalism (panels); Availability of trained technicians | ||
| + | | None | ||
| + | | Small Loads; Areas where fuel is costly or difficult to obtain | ||
| + | |- | ||
| + | | '''Wind Turbine with Batteries''' | ||
| + | | High | ||
| + | | Low-moderate | ||
| + | | High (if maintained properly) or low (if not) | ||
| + | | 20 years (turbine), 10 years (blades), 5 years (batteries) | ||
| + | | Theft (batteries); Lack of data on wind resources | ||
| + | | None | ||
| + | | Many moderate loads where resource is sufficient | ||
| + | |- | ||
| + | | '''Diesel Generator''' | ||
| + | | Moderate-high | ||
| + | | High | ||
| + | | High | ||
| + | | 25,000 operating hours | ||
| + | | Fuel spills; emissions | ||
| + | | Very High | ||
| + | | Larger loads | ||
| + | |- | ||
| + | | '''Gasoline Generator''' | ||
| + | | Low | ||
| + | | Very High | ||
| + | | Moderate | ||
| + | | 1,000 - 2,000 operating hours | ||
| + | | Fuel spills; emissions; flammability | ||
| + | | High | ||
| + | | Emergency Generator | ||
| + | |- | ||
| + | | '''Gas Generator''' | ||
| + | | Moderate | ||
| + | | High | ||
| + | | Moderate | ||
| + | | 3,000 operating hours | ||
| + | | Propane is of limited availability, but can use biogas | ||
| + | | Low | ||
| + | | Component in hybrid system or stand-alone | ||
| + | |- | ||
| + | | '''Hybrid System''' | ||
| + | | Very high | ||
| + | | Low-moderate | ||
| + | | Very High | ||
| + | | Varies; optimization greatly extends generator and battery life | ||
| + | | Complexity for servicing | ||
| + | | Low | ||
| + | | Medium and large loads | ||
| + | |- | ||
| + | | '''Grid extension''' | ||
| + | | Varies | ||
| + | | None | ||
| + | | Varies | ||
| + | | High | ||
| + | | Theft; extending grid allows connection of nearby homes to grid | ||
| + | | Not local | ||
| + | | Where grid is reliable and not too distant | ||
| + | |} | ||
| + | |||
| + | <br /> | ||
| + | |||
| + | ==== Costs of Different Technologies ==== | ||
| + | |||
| + | In general, renewable energy options will have higher capital costs than diesel or other fuel-based electricity generating options. However, in the long run, renewable systems will have lower operating costs and produce fewer or no emissions. In renewable energy systems, battery maintenance, occasional cleaning, and theft-prevention will be the major recurring costs. A hybrid system using an alternative energy source (e.g. PV system) and a traditional generator (e.g. diesel) will have higher up-front capital costs than a renewable-only system; however, hybrid systems provide greater flexibility, including the ability for one system to support the other.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> | ||
| + | |||
| + | A detailed list of costs of power sources for different health clinic categories can be found in the USAID publication “[https://pdf.usaid.gov/pdf_docs/PNADJ557.pdf Powering Health]”.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref><br /> | ||
| + | |||
| + | |||
| + | === System Sustainability === | ||
| + | |||
| + | To ensure a reliable electricity supply in the long run, not only quality equipment is needed when the system is set up: maintenance and repairs, secured finance of operation and maintenance, as well as professional organizational management is of high relevance, too. | ||
| + | |||
| + | ==== Maintenance ==== | ||
| + | |||
| + | Regular and timely maintenance is essential to proper functioning of the equipment. Off-grid technologies often fail pre-maturely due to lack of maintenance, leading to the perception that renewable technologies are too unreliable to serve the needs of communities. According to a study by the World Bank (2017), it is estimated that many PV systems become inoperative after 3–5 years if maintenance and repair services are not provided.<ref name="World Bank (2017): State of Electricity Access Report, Special Feature - Modern Energy Access and Health. http://documents.worldbank.org/curated/en/756131494939083421/pdf/BRI-P148200-PUBLIC-FINALSEARSFHealthweb.pdf">World Bank (2017): State of Electricity Access Report, Special Feature - Modern Energy Access and Health. http://documents.worldbank.org/curated/en/756131494939083421/pdf/BRI-P148200-PUBLIC-FINALSEARSFHealthweb.pdf</ref> | ||
| + | |||
| + | Maintenance challenges include:<ref name="World Bank (2017): State of Electricity Access Report, Special Feature - Modern Energy Access and Health. http://documents.worldbank.org/curated/en/756131494939083421/pdf/BRI-P148200-PUBLIC-FINALSEARSFHealthweb.pdf">World Bank (2017): State of Electricity Access Report, Special Feature - Modern Energy Access and Health. http://documents.worldbank.org/curated/en/756131494939083421/pdf/BRI-P148200-PUBLIC-FINALSEARSFHealthweb.pdf</ref><ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> | ||
| + | |||
| + | *Routine maintenance and cleaning needs to be done regularly | ||
| + | *Routine maintenance as well as major overhauls and capital replacement need to be planned and budgeted for in advance | ||
| + | *Lack of funding for spare parts | ||
| + | *Lack of local qualified technicians | ||
| + | *Emergency back-up generators should be checked periodically even if rarely used | ||
| + | *Improper or insufficient maintenance can lead to substantial costs in the future | ||
| + | |||
| + | Regular maintenance is well worth the cost, and programs installing energy systems at health clinics or other facilities should ensure there will be a commitment to servicing the system. Experts recommend training local personnel in the servicing of these systems or obtaining a long-term maintenance contract with a service provider.<br /> | ||
| + | |||
| + | |||
| + | ==== Financing of Operation and Maintenance ==== | ||
| + | |||
| + | Financing of renewable energy system use and maintenance, including component replacements, is key to system sustainability in the long run. Oftentimes the most difficult question to resolve is how to pay for component replacements, from light bulbs to batteries.<ref name="ESMAP 2010: Photovoltaics for Community Service Facilities http://documents.worldbank.org/curated/en/837791468332067596/pdf/632250WP0Photo00Box0361508B0PUBLIC0.pdf">ESMAP 2010: Photovoltaics for Community Service Facilities http://documents.worldbank.org/curated/en/837791468332067596/pdf/632250WP0Photo00Box0361508B0PUBLIC0.pdf</ref> A lack of funding for operating and maintenance can result in unusable equipment. | ||
| + | |||
| + | Clinic managers must develop a sustainable way to pay for the maintenance and operation of the system to ensure continuity of facility operations. Facilities could consider incorporating aspects of the finance structures described below by USAID into their financial and operating practices.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> | ||
| + | |||
| + | <u>'''User Fees'''</u> | ||
| + | |||
| + | A “user fee” system involves building the cost of energy into the overall cost of medical services – passing the cost to the patient. Most rural healthcare facilities struggle to secure sufficient operating funds due to the inability to pass along true costs of medical service to users who lack the resources to pay actual costs. The inability of patients to pay, coupled with the challenge of managing the collection and disbursement of funds, makes this approach difficult to implement.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> | ||
| + | |||
| + | <br/><u>'''Sale of Excess Electricity'''</u> | ||
| + | |||
| + | The sale of excess electricity offers a promising approach to finance operations. By installing a mini-grid system with excess capacity, income from the sale of additional electricity can offset a portion, if not all, of the system’s operating costs. | ||
| + | |||
| + | *Bulk (Wholesale): By operating the power system as a small enterprise, excess electricity can be sold to nearby villages, factories, schools or facilities. The system must be sized to accommodate both the clinic and the potential customer base. Customers must be in close proximity to the system or transmission costs quickly make this approach prohibitively expensive. Maintenance requirements are also more complex, thus budgets to be planned in need to be higher.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> Insufficient interaction between medical, building and engineering staff, and utilities can be another barrier for leveraging the electricity generation potential of health facilities for broader community needs. Careful planning and capacity building is necessary.<ref name=":0" /><ref name="WHO, The World Bank (2015): Access to modern energy services for health facilities in resource-constrained settings: a review of status, significance, challenges and measurement. https://apps.who.int/iris/bitstream/handle/10665/156847/9789241507646_eng.pdf%3Bjsessionid=05BA6EDD62617D7CFB7AE8FBE47A639A?sequence=1">WHO, The World Bank (2015): Access to modern energy services for health facilities in resource-constrained settings: a review of status, significance, challenges and measurement. https://apps.who.int/iris/bitstream/handle/10665/156847/9789241507646_eng.pdf%3Bjsessionid=05BA6EDD62617D7CFB7AE8FBE47A639A?sequence=1</ref> | ||
| + | *Point of Use Sale (Retail): When potential purchasers of power are too remote to obtain the electricity over transmission lines, the clinic can sell it at or near their facility. A small powering station can be established with fees charged based on the amount of power used, if metering is available, or according to time. For customers with transportable devices such as power tools, a small work area with outlets can be set aside adjacent to the power station where users can plug in equipment. Villagers can use these areas for income-generating activities. It may be feasible to establish a “mini industrial zone” near the clinic’s power system, providing an area with permanent workshops (sewing, weaving or repair services) or stores. The clinic could realize income from rent on the workshop/store space, the sale of electricity, and the pumping of water.<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> | ||
| + | '''<u>Productive Uses within the health center premises</u>''' | ||
| + | |||
| + | Using the excess electricity for productive uses like running a canteen/restaurant, offering phone charging, sale of cold drinks/food requiring refrigerations within the health center premises can serve as a potential source of income for O&M of the solar systems. GIZ Uganda is piloting this model in health centers in displacement settings in Uganda in 2021/2022. <ref>Electrification of Health Centers in Displacement Settings: https://energypedia.info/images/8/8a/Electrification_of_Health_Centers_in_Displacement_Setting.pdf | ||
| + | |||
| + | [[Webinar Series on Decarbonisation of Energy Infrastructure in Displacement Situations]]</ref> | ||
| + | |||
| + | | ||
| + | |||
| + | ==== Institutional Management ==== | ||
| + | |||
| + | As the finance provider, the system installer, and system owner are almost always different actors, clear arrangements are needed regarding a division of responsibilities, ownership and accountability to keep the energy system functioning. Lacking ownership or capability of institutions can be encountered by careful planning, stakeholder engagement, sensitization, and capacity building to achieve organizational sustainability.<ref name="UN Foundation, SEforALL (2019): Lasting impact – Sustainable off-grid solar delivery models to power health and education. http://poweringhc.org/wp-content/uploads/2019/04/Lasting-Impact_Sustainable-Off-Grid-Solar-Delivery-Models-to-Power-Health-and-Education.pdf">UN Foundation, SEforALL (2019): Lasting impact – Sustainable off-grid solar delivery models to power health and education. http://poweringhc.org/wp-content/uploads/2019/04/Lasting-Impact_Sustainable-Off-Grid-Solar-Delivery-Models-to-Power-Health-and-Education.pdf</ref> Having an entity that has a stake in the continued successful operation of the system is crucial to cultivating a sense of ownership for ongoing system operation. | ||
| + | |||
| + | | ||
| + | |||
| + | == Stepwise Approach to Electrifying a Health Center == | ||
| + | |||
| + | According to USAID:<ref name="USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf">USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf</ref> | ||
| + | |||
| + | #'''Identify the Health Center's Current Energy Demands'''<br/>Identify current energy needs and applications, e.g. for lighting, refrigeration, communication, etc. | ||
| + | #'''Account for Near-Term Change'''<br/>Determine whether energy demands will change in the near-term. | ||
| + | #'''Establish Target Energy Consumption in kWh/day'''<br/>Use tools such as the USAID [http://tools.poweringhealth.org/ Health Clinic Power System Design Tool] (4 - Electric Load Inputs) or the [http://www.poweringhealth.org/index.php/resources/tools/energy-audit-spreadsheet Energy Audit Spreadsheet] (Worksheet 7 - Future Electric Applications) to calculate the future electric energy consumption in kWh/day. | ||
| + | #'''Determine Technologies Needed to Meet Target'''<br/>Evaluate energy technologies. | ||
| + | #'''Procure, Design System, and Install Technology'''<br/>Select the most appropriate energy technology. | ||
| + | #'''Maintain and Financing Your Energy Technology'''<br/>Institute financing mechanism(s) accounting for operation and maintenance needs and costs. | ||
| + | |||
| + | Remember to contact an expert for assessment, system design, procurement, installation, and maintenance of energy technologies! | ||
| + | |||
| + | |||
| + | == Thermal Energy for Health Facilities == | ||
| + | |||
| + | In addition to electricity, health facilities need thermal energy for food preparation, water and space heating, sterilization of equipment and medical waste incineration. Also for cooling in applications such as absorption refrigeration (using LPG or kerosene), thermal energy may be used. | ||
| + | |||
| + | In general, there is little focus and information on thermal energy demand and supply of health facilities to be found in literature and studies. | ||
| + | |||
| + | In settings, where access to electricity is no problem, some or all thermal needs may be met with electric-powered appliances. However, very often the reality of rural health centers is different: thermal energy is mainly produced through direct combustion of fuel, e.g. firewood or charcoal, gas, kerosene or diesel.<ref name=":0" /> | ||
| + | |||
| + | === Food Preparation === | ||
| + | |||
| + | In most rural health facilities, thermal energy is needed for food preparation – for staff as well as for patients. | ||
| + | |||
| + | ==== Food for Staff ==== | ||
| + | |||
| + | It depends mainly on the number of staff, the health center management and/or the degree of self-organization of the staff if the meals for staff members are prepared communally. In this case an institutional size stove might make sense.<br/> | ||
| + | |||
| + | Examples: Both Mission and the Government hospitals in Mulanje District (Southern Malawi) have institutional size wood-fired rocket stoves to cater for the staff and the students of the nursing college. Cooking is done by a paid cook, who got trained by GIZ on the proper use of the stoves. The firewood is provided by the hospital. Savings as compared to the open fire are between 70-80 percent. | ||
| + | |||
| + | ==== Food for Patients ==== | ||
| + | |||
| + | Most rural health centers do not provide meals for the patients, even if they have in-patient facilities. Usually, the meals for patients are prepared individually by the guardians who accompany the patient often with the main purpose to cater or prepare warm bath water for the patient. Thus individual cooking facilities are needed for the guardians. Usually food ingredients, fuel and cooking utensils have to be organized by the guardians and are not provided by the health center. Thus the most prevalent cooking facility is the 3-stone fire fueled with firewood or any other biomass that the guardians are able to organize in the immediate surroundings of the health center. A good practice is when health centers provide a sheltered cooking place and define the area where cooking is allowed. To minimize the adverse effects of air pollution and prevent that smoke is adding to the ailments of the patients, this location should preferably be at a distance from the wards and care units. | ||
| + | |||
| + | Mulanje Mission Hospital in Southern Malawi went even further: they had already a roofed kitchen for the guardians with 20 simple fireplaces. As hospital facilities were expanding and the number of in-patients increasing, the kitchen became too small. With advice from GIZ-project staff on stove technology and kitchen design, they added another roofed kitchen with improved fixed ‘Esperanza’ -type stoves and good ventilation. In the first weeks the kitchen was not yet well accepted and rather empty, because people were not familiar with the stoves and were unsure how to use them. Upon realizing this, a permanent security staff of the hospital got trained on the correct stove use and was able to show the ever-changing users, who normally don’t use the kitchen longer than a few days. From then onward the kitchen became more and more popular as people became aware of the advantages: the new stoves were more economic, cooked faster, created less smoke, and the building had a better ventilation. Young mothers felt more comfortable bringing their babies in the new kitchen. The challenge is to organize the maintenance of the stoves, as some of the ceramic pot-supports of the ‘Esperanza stoves’ had gone missing and the stoves performed poorly without them. | ||
| + | |||
| + | |||
| + | === Sterilization / Pasteurization / Water Heating === | ||
| + | |||
| + | Thermal energy is also needed for the sterilization of instruments, the pasteurization of drinking water and to heat bath water for the patients. Thermo-solar energy might be an option, if used with a (reusable) temperature indicator to ensure that the water has reached the required temperature. Solar energy is also a good option to heat bath water for the patients, if storage of hot water is provided. Conventional passive solar thermal water heating systems are becoming more common in developing countries, and can usually heat water to a temperature suitable for basic hygiene and sanitation.<ref name=":0" /> | ||
| + | |||
| + | |||
| + | == Space Heating == | ||
| + | |||
| + | Space heating is important in health facilities in temperate climates, and during the cold season of higher-altitude zones of Central Asia, Latin America and Africa, as well as the Mediterranean. | ||
| + | |||
| + | Space heating in developing-country health facilities may be provided by district heating, electricity or on-site fuel-based solutions. Inexpensive thermal solar panels can also provide hot water for space heating. | ||
| + | |||
| + | Improving the energy efficiency of buildings can greatly reduce thermal energy needs as well as electricity requirements.<ref name=":0" /> | ||
| + | |||
| + | | ||
| + | |||
| + | == Project Experience == | ||
| + | |||
| + | * Experience and lessons learned, including project approaches, technical details and evidence for impacts of GIZ projects in [[Uganda Energy Situation|Uganda]] and [[Ethiopia Energy Situation|Ethiopia]] are discussed in the [[Photovoltaic (PV) for Health Centers - Project Experience|article "Photovoltaic (PV) for Health Centers - Project Experience"]]. It aims at compiling experience from past and ongoing PV programmes for rural health centers. | ||
| + | * '''Sustainable energy access for social institutions through service models''' | ||
| + | |||
| + | According to surveys conducted by the Green People’s Energy (GBE, Grüne Bürgerenergie) Benin project between 2020–2021, more than 69% of the solar systems installed up to five years prior by various electrification efforts (donors, government, charities) in health centers were no longer functioning. In order to ensure the sustainability of solar systems installed for the benefit of social institutions, the German cooperation-financed GBE Programme implemented by GIZ, pilots service-based delivery models in Benin that are based on a long-term commitment of a service provider (i.e. a solar company) to maintain the system and of the client (i.e. the social institution) to pay a monthly fee. | ||
| + | |||
| + | Read more about this approach [[Sustainable energy access for social institutions through service models|here]]. | ||
| + | |||
| + | * '''Improving Health Services for the Rural Population in Ghana''' | ||
| + | |||
| + | A project by the Green People’s Energy (Grüne Bürgerenergie, GBE) aims at improving the conditions for rural communities to use renewable energy applications in their social infrastructure by supporting 31 clinics. The clinics were selected by the Ghana Health Service, the state-owned agency responsible for the operation and maintenance of around 500 rural clinics in Ghana, jointly with the Ministry of Energy and GBE. | ||
| + | |||
| + | Read more about the project and its lessons learned [[Improving Health Services for the Rural Population in Ghana|here]]. | ||
| + | |||
| + | * '''Improved Energy Access for the Kaffrine Region''' | ||
| + | |||
| + | Kaffrine is a rural region in Senegal where more than half of the population and social institutions (e.g. schools and health posts) do not have access to electricity from the national grid. The GBE project supports the acquisition, sustainable management, and financial viability of solar systems for the benefit of ten rural sewing craft enterprises, eight schools and five health centres in Kaffrine. | ||
| + | |||
| + | Read more about the project [[Improved Energy Access for the Kaffrine Region|here]]. | ||
| + | |||
| + | == Further Information == | ||
| + | |||
| + | *[[Webinar Series: Sustainable Energy in Humanitarian Settings|Webinar on Powering Humanitarian Health Operations: Sustainable Energy Solutions]] | ||
| + | *Articles on energypedia: | ||
| + | **[[Access to modern energy and the impact on health|Access to modern energy and the impact on health]] | ||
| + | **[[Photovoltaic (PV) for Health Centers - Project Experience|Project Experience with PV for Health Centers]] | ||
| + | **[[Electrification of Social Institutions with Solar Photovoltaic -Lessons Learned from Uganda|Electrification of Social Institutions with Solar Photovoltaic - Lessons Learned from Uganda]] | ||
| + | |||
| + | *SEforAll, The World Bank (2021): [https://www.seforall.org/system/files/2021-07/PHC-solutions-catalogue-v7-SEforALL.pdf Powering Healthcare Solutions Catalogue.] | ||
| + | *[http://www.poweringhealth.org/ Powering Health, USAID website] covering all major issues on electricity supply for rural health centers. Several country case studies available. Offers tools for energy audits and load calculation. Highly recommandable! | ||
| + | *USAID: [http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf Powering Health: Electrification Options for Rural Health Centers] - Step-by-step guide on energy needs, power generation options, and sustainability issues for rural health centers. Case studies from Botswana and Uganda. | ||
| + | *[https://www.esmap.org/ ESMAP] (2010): [http://siteresources.worldbank.org/EXTAFRREGTOPENERGY/Resources/717305-1266613906108/PV_Toolkit_FINAL_12-14-10.pdf Photovoltaics for Community Service Facilities]". This very resourceful handbook covers the most relevant issues regarding sustainability and long-term operation of community PV systems. | ||
| + | *Practical Action (2007): [http://answers.practicalaction.org/our-resources/item/solar-photovoltaic-refrigeration-of-vaccines Solar PV Refrigeration of Vaccines] - Technical Background of solar refrigeration | ||
| + | *IEA (2014): [[:File:PV Systems for Rural Health Facilities in Developing Areas.pdf|PV Systems for Rural Health Facilities in Developing Areas.pdf]] | ||
| + | *National Renewable Energy Laboratory USA (1998): [https://www.nrel.gov/docs/legosti/fy98/25233.pdf Renewable Energy for Rural Health Clinics]- Publication on energy issues of rural health clinics: energy applications, electrical system components, system selection and economics, institutional considerations. Also provides case studies and lessons learned. | ||
| + | *The World Bank (2020): [https://openknowledge.worldbank.org/bitstream/handle/10986/33276/Increasing-Human-Capital-by-Electrifying-Health-Centers-and-Schools-through-Off-Grid-Solar-Solutions.pdf?sequence=1&isAllowed=y Increasing Human Capital by Electrifying Health Centers and Schools through Off-Grid Solar Solutions.] Live Wire Brief 2020/104 | ||
| + | *IRENA, UNSD, World Bank, WHO. 2020. [https://trackingsdg7.esmap.org/data/files/download-documents/02-sdg7-chapter1-accesstoelectricty_0.pdf Tracking SDG 7: The Energy Progress Report. Chapter 1 Access to Electricity.] | ||
| + | |||
| + | |||
| + | == References == | ||
<references /> | <references /> | ||
| + | |||
| + | [[Category:Energy_Access]] | ||
| + | [[Category:WASH]] | ||
| + | [[Category:Rural_Electrification]] | ||
| + | [[Category:Energy_Use]] | ||
| + | [[Category:Impacts_Health]] | ||
Latest revision as of 13:25, 14 September 2023
Introduction
Health professionals in rural clinics face many challenges on a daily basis. Not only a lack of qualified medical staff, equipment and medicine can become a major obstacle in providing crucial basic health services for the rural population, also lacking or unreliable energy supply can be a severe problem.
If the cold chain is inoperable when supplies arrive, vaccines, blood, and other medicines may go to waste. Without proper electric lighting, most medical treatments can only be conducted at daytime, while emergency surgeries at night may only be illuminated by dim kerosene lamps or torches. Also for the provision of water, energy is frequently required for pumping and heating.
Despite its high relevance for the provision of health services, there is little reliable data on energy access in health facilities in developing countries.
In India, Rural Health Statistics 2018 data showed nearly 22% or 40,000 primary health centers in rural India are still operating without electricity supply.[1]
A review led by the World Health Organization (WHO) in 2013 found nationally representative data for only 14 developing countries globally, 11 of them in sub-Saharan Africa. According to this review, one in four health facilities in Sub-Saharan Africa had no access to electricity, while only 28% of health facilities and 34% of hospitals had reliable access to electricity.[2]
A recent survey of 78 countries found that only 41% of low- and middle-income country health care facilities have reliable electricity.[3]
This is not only hampering proper medical services, electricity outages also can damage medical and diagnostic devices.
In addition to electricity, health facilities need thermal energy for cooking, heating, and sterilization. This demand is mostly met by direct combustion of fuels like kerosene, diesel, biomass or gas.
The widespread use of fossil fuels like kerosene for lighting or diesel for power generation, as well as biomass in inefficient cookstoves cause additional risks to staff, patients and the environment due to emission of particulate matter, black carbon and CO2, and fire hazards.[2]
Selecting appropriate sources of reliable and sustainable energy as well as introducing measures for efficient energy consumption can help mitigate some of the challenges inherent in operating a health facility in the developing world.
This article will provide an overview on options for the improvement of the energy situation in rural health facilities.
Electricity in Healthcare Facilities
Health facilities have different energy needs according to their services provided and on consequently required loads. Some of the basic services include vaccine refrigeration, light, medical equipment, and surgical treatment. Further services include e.g. communication, water pumping and heating, space heating or cooling.
Successful development of reliable energy systems requires careful assessment of all aspects of health facility energy needs, including both electric and thermal energy needs.
Growing energy needs and foreseeable load increases in the near future also need to be considered when analyzing and determining a facility’s load profile. Procurement of more or less energy-efficient medical equipment will influence the future load profile, as will energy-saving retrofits to the building itself. For more information about building efficiency, see WHO/World Bank 2015.[2]
Classification of Health Facilities
Healthcare posts and clinics can be distinguished into three categories, namely low, medium, and large health facilities with different energy requirements accordingly.[4][5][6]
Health posts are the smallest, most basic facilities. These locations typically will not have a permanent doctor or nurse on staff. They provide basic treatment for emergency cases, first aid, and where possible, basic immunization services. Due to the limited medical equipment used, the overall energy demand of health posts is relatively low. The energy demands of a health post is similar or less than that of a small health clinic.
Health clinics are generally larger than health posts and employ one or more full-time nurses. A health clinic offers a wider array of services than a health post and will possess equipment allowing for more sophisticated diagnoses. Rural health clinics generally fall into one of three categories (Categories I, II and III - see table below) based on the type and number of medical devices used in the facility and the frequency with which they are used on a daily basis. Local resources may make specific energy options more or less advantageous in each location.
The IEA describes the example of a ‘typical’ electrical load distribution of a small health facility in Cambodia (based on PV provision) as 35% lights, 14% fans, 34% lab equipment and 17% other, with the load curve increasing gradually to a midday peak and then decreasing gradually.[4]
Another example load profile of a medium size health facility shows that the highest energy consumption within day time is by laboratory equipment, while lighting systems and fans consume more during the night. The overall electricity distribution, however, shows that the main consumers are lighting systems and fans (57%), followed by lab equipment (29%) and other equipment (14%).[4]
Other types of health facilities that require reliable and sustainable electrification include blood banks, stand-alone laboratories and pharmacies, and anti-retroviral treatment (ARV) clinics. Blood banks, stand-alone labs, and pharmacies will, depending on their size, utilize equipment similar to that found in small or medium sized health clinics and will have similar energy needs. ARV clinics will have significant energy demands similar to those found large-sized health facilities.[5]
| Category | Description |
|
Category I low energy requirements, 5 - 10 kWh/day |
Electric power is required for:
|
|
|
37 health clinics were electrified with off-grid solar systems, consisting of 800Wp Solar Panels, 2.5kWh Lithium batteries (LiFePO4) and 800VA inverter. Each health clinic has around 20 lights (both indoor and outdoor) and sockets have been provided to power basic lab equipment or for powering laptops if necessary. Each system can provide on an average 3-4kWh of clean energy per day. Click here for more! |
|
Category II moderate energy requirements, 10 - 20 kWh/day |
Electric power is required for:
|
|
|
Close to 50 health centers have been electrified so far in Malawi. One of the key problems of not having reliable power at health centers is high attrition rates with healthcare staff preferring urban health centers with better facilities. Realizing this problem, we connected staff quarters with the solar off-grid energy system. Each of these systems ranged from 5-20kWp depending on the size and capacity of the health center. This solved two main problems: Basic amenities for the staff and additional revenue from selling excess energy towards maintenance of the systems. These systems are remotely monitored for preventive maintenance, visits are planned every six months, and staff is professionally trained to operate and use the system. Click here for more! |
|
Category III Large-sized health facility/ District or Regional hospitals high energy requirements, 20 - 30 kWh/day |
Electric power is required for:
|
|
|
Close to 450kWh lithium batteries and 220kWp PV are installed at 6 rural health units (RHUs) and 2 district hospitals in Mindanao region of Philippines. Reducing the diesel consumption to a minimum (even to zero at some hospitals), cuts fuel expenses and carbon emissions and at the same time provides reliable energy services 24/7. The project is done for International Organisation for Migration (IOM) and financed by the Government of Japan. These hospitals offer range of services, from complex surgeries to diagnostics. Solar systems are powering everything, from sophisticated diagnostic equipment to communications (computers and internet) and also staff quarters. |
Electricity Needs
Some very common and basic devices or services that need electricity are the following:
Vaccine refrigeration
While refrigerators work 24h/day, they actually do not continuously consume power. To keep the internal temperature constant, the compressor or heater runs in a controlled duty cycle mode. Therefore, in order to obtain information about the daily energy demand of a refrigerator, the device's duty cycle must be determined (e.g. by listening), or by measuring the energy consumption for a period of time.[4]
Lighting
This is a very essential service in rural health facilities, mainly at night. Quality and availability of light significantly improves medical emergency interventions, including first aid, birthing and surgery.[4]
Medical equipment
A microscopes is an essential equipment in rural health facilities. In developing countries, common diseases which include HIV, syphilis, malaria, and anemia are diagnosed using a microscope.[4]
Sterilization
Medical tools, including surgical equipment need to be sterilized. Often, sterilization of equipment by air requires a high temperature up to 160◦C for around two hours, while steam autoclaves, where a temperature of 120◦C is sufficient, are even more effective. Because of the required high temperature, sterilization equipment consumes a considerable amount of energy.[4]
Basic Needs Assessment
When considering the type of electrification needed to sustain daily operations, a facility must first understand its basic needs. The needs assessment will include an inventory of the types of equipment used in the facility and the power required to operate each device. Understanding the average “daily load”, or the amount of power required to operate equipment under normal working conditions, will influence the choice of power supply. Once the daily energy demand is established, a range of electrification options can be considered. Understanding the need will also provide managers with a realistic budget for procuring, installing, and maintaining the new system.
Additionally, when determining how to electrify a healthcare facility, it can also be important to prioritize the electrification of equipment based on its criticality to patients’ survival and the facility’s operation. A. Franco et al. (2017)[7] propose three categories: non-critical, non-secured and secured. Non-critical refers to equipment that is not critical to patient survival, such as air ventilation in the ward. Non-secured refers to equipment that is critical but can handle moderate voltage fluctuations of the network and short outages, often thanks to an integrated battery. Finally, secured refers to equipment that is critical and needs to be protected against voltage fluctuations. During a power shortage, this prioritization can help in effectively managing electricity production and consumption.
The table below shows a list of common health facility equipment and their respective power needs.[7]
For further information about power requirements of electrical devices for health services see also tables 3 and 4 in the publication “Access to Modern Energy Services for Health Facilities in Resource-Constrained Settings” from WHO / World Bank 2015.[2]
Tools for Calculating Electricity Needs of a Health Facility
The USAID Health Clinic Power System Design Tool (4 - Electric Load Inputs) and/or the Energy Audit Spreadsheet (Worksheet 7 - Future Electric Applications) as well as the examples of energy demands of typical rural health centers in developing countries can help identifying the overall energy demands of health facilities. The amount of expected energy consumption in kWh/day, in addition to expert consultation, will assists in the selection of appropriate electrification technology.
Once a facility has comprehensively analyzed the energy requirements of its day-to-day operations, likely changes of those demands should be considered. Facility managers must think strategically about the possibility that energy demands may increase due to the addition of patients, extended operating hours, or new services. Once this process has been completed and an adequate accounting of needs has been made, the manager can determine the various energy options to meet those demands. These options must be considered in light of all facility-specific variables.
Electricity Supply Options
Once the daily energy demand has been assessed, the next step is evaluating the potential technical solutions for providing sustainable energy services. In areas where access to the national grid electricity infrastructure is available and reliable, this is usually the primary energy source. Wherever this is not the case, off-grid energy systems and on-site power generation solutions must be taken into account. Off-grid energy systems include i.e. generators, renewable energy systems (fueled by solar power, wind power, micro-hydro power), batteries or a combination of two or more of the above-mentioned technologies. The best option for a given application depends on a number of factors, and in some cases a combination of power supply options may be the best solution.
Some factors to consider include:[5]
Reliability of local grid
Local renewable energy resources (wind, solar, water)
Local availability of conventional energy sources (diesel, propane, gasoline)
Local capital cost and operating cost
Local availability of systems, parts, service companies, and technicians
Governmental policies and incentives
System reliability requirements
Technical capacity and funds for system maintenance and replacement
Emissions
Special considerations or desired operational characteristics - i.e. noise, etc.
Technological Options
- Generators
Generators run on various fuels, including natural gas, diesel, gasoline and propane. They have been the default onsite power option for a long time, typically powering off-grid facilities. They are also the most widespread back-up energy source for healthcare facilities in the Global South, even for grid-connected facilities.[7]
The advantage of generators is that they use a consolidated technology with low upfront capital costs. Disadvantages compared to renewables are increasing fuel costs and unstable fuel supply to remote areas (especially in rainy seasons) as well as the role fossil fuels play in global warming.
- Photovoltaic (PV)
Photovoltaic (PV) Systems generate electricity from sunlight collected by solar panels. Energy collected this way can be used to supply direct power to electrical equipment, or it can be stored in batteries to provide indirect power. In combination with a battery, PV systems are excellent for handling small-to-moderately sized loads in locations where grid electricity is not available. They are highly modular, so it is easy to customize the system to the needs of a facility and add units if power demand increases.
As PV converts solar energy to direct-current (DC), photovoltaic systems must be equipped with inverters in order to convert the DC power input to alternating-current (AC) power. Alternatively, devices have to run directly on DC, which is already very common for refrigerators.
In many developing countries harnessing the power of the sun is already widespread for electricity generation. Sharply declining costs, local availability and no emittance of greenhouse-gas emissions makes PV are real alternative to fossil-fueled generators. Standalone solar PV solutions are currently the dominant model for electrifying public institutions, such as health facilities.[8]
Find more info on PV in our solar portal on energypedia.
A very helpful tool, the Global Solar Atlas, with worldwide solar irradiation data per country and region is provided by the World Bank.
- Wind Energy
Depending on the geographical location, wind can be an abundant source of energy. Situating a wind turbine on a site requires careful measurement of wind patterns. Mini and small wind turbines ranging from 1 to 100 kW are mainly used for off-grid rural electrification and can be used in homes and in small communities. Medium and large size wind turbines with capacities ranging from 100 kW to several mega-watts can be used both for on-grid electrification (through connection to the main grid) or off-grid electrification.
Small wind turbines with a diameter of less than 15 m (usually 7 m) require relatively low wind speeds (typically between 3 and 4 meters per seconds, or m/s) for activation, and can thus be employed as an energy source in off-grid healthcare facilities.[7]
Similar to PV systems, wind turbines must be connected to the grid or to a battery system to provide reliable power.
Find more info on wind energy in our wind portal on energypedia.
A very helpful tool to identify high-wind areas per country and region is the Global Wind Atlasprovided by the World Bank.
- Micro / Pico Hydro
In water-rich off-grid settings, micro- and pico-hydropower could also be used for the electrification of healthcare facilities. Micro-hydropower refers to power capacity from 5 kW up to 100 kW, and pico-hydro (up to 5 kW).[9] This renewable, clean energy is not intermittent, like solar and wind, though comparable in terms of investment costs. It is the preferred choice for water-rich regions in countries such as Ethiopia, Uganda, Rwanda and the Democratic Republic of Congo.[7]
Find more info on micro and pico hydro energy in our hydro portal on energypedia.
- Hybrid Systems
Hybrid-energy systems can include a generator, a PV and/or wind installation and/or hydropower and batteries. This way, limitations of each power system can be overcome and benefits maximized.
With reliable solar and wind resources, a hybrid system will rarely need to rely on a generator. However, it can serve as a backup in case of bad weather. Since the generator can recharge the batteries during prolonged periods of inclement weather, the battery bank in a hybrid system can be significantly smaller than in a PV-battery system, perhaps storing only one or two days’ worth of energy. The low duty cycle minimizes operation costs and extends generator lifetime.[5][7]
- Mini-grids
- Grid Extension
Grid extension connects the health facility to the local utility. Cost depend on the utility, the terrain, the distance to be covered, and the size of the load to be served. If the local grid is fairly reliable and within a few miles, obtaining an estimate for the capital cost of grid extension and the recurring cost of electricity will give points of comparison when considering other options.
Grid extension typically has a high capital cost, but offers several advantages. First, in most cases, the cost varies only slightly with the size of the load to be served. This makes it uneconomical for small loads but a better option for large loads. Second, once the grid has been extended to the clinic, it can serve other local loads. Third, operations and maintenance are the responsibility of the utility.[5]
Electricity Technology Characteristics
The table below from USAID (no date, probably published between 2006 and 2010) illustrates the key characteristics of some energy generation technologies. Please keep in mind that costs of renewable energy systems have decreased significantly over the last years, so the assessment provided in the table might have changed. It is also highly dependent on local circumstances, for example import taxes or domestic production, and international fuel prices.
| Energy Technologies | Capital Cost | O&M Cost | Reliability | Durability | Special Considerations | Emissions | Optimal Use |
|---|---|---|---|---|---|---|---|
| Solar PV System with Batteries | Very high | Low | High (if maintained properly) or low (if not) | 20-30 years (PV), 5 years (batteries) | Theft (batteries or panels); Vandalism (panels); Availability of trained technicians | None | Small Loads; Areas where fuel is costly or difficult to obtain |
| Wind Turbine with Batteries | High | Low-moderate | High (if maintained properly) or low (if not) | 20 years (turbine), 10 years (blades), 5 years (batteries) | Theft (batteries); Lack of data on wind resources | None | Many moderate loads where resource is sufficient |
| Diesel Generator | Moderate-high | High | High | 25,000 operating hours | Fuel spills; emissions | Very High | Larger loads |
| Gasoline Generator | Low | Very High | Moderate | 1,000 - 2,000 operating hours | Fuel spills; emissions; flammability | High | Emergency Generator |
| Gas Generator | Moderate | High | Moderate | 3,000 operating hours | Propane is of limited availability, but can use biogas | Low | Component in hybrid system or stand-alone |
| Hybrid System | Very high | Low-moderate | Very High | Varies; optimization greatly extends generator and battery life | Complexity for servicing | Low | Medium and large loads |
| Grid extension | Varies | None | Varies | High | Theft; extending grid allows connection of nearby homes to grid | Not local | Where grid is reliable and not too distant |
Costs of Different Technologies
In general, renewable energy options will have higher capital costs than diesel or other fuel-based electricity generating options. However, in the long run, renewable systems will have lower operating costs and produce fewer or no emissions. In renewable energy systems, battery maintenance, occasional cleaning, and theft-prevention will be the major recurring costs. A hybrid system using an alternative energy source (e.g. PV system) and a traditional generator (e.g. diesel) will have higher up-front capital costs than a renewable-only system; however, hybrid systems provide greater flexibility, including the ability for one system to support the other.[5]
A detailed list of costs of power sources for different health clinic categories can be found in the USAID publication “Powering Health”.[5]
System Sustainability
To ensure a reliable electricity supply in the long run, not only quality equipment is needed when the system is set up: maintenance and repairs, secured finance of operation and maintenance, as well as professional organizational management is of high relevance, too.
Maintenance
Regular and timely maintenance is essential to proper functioning of the equipment. Off-grid technologies often fail pre-maturely due to lack of maintenance, leading to the perception that renewable technologies are too unreliable to serve the needs of communities. According to a study by the World Bank (2017), it is estimated that many PV systems become inoperative after 3–5 years if maintenance and repair services are not provided.[10]
Maintenance challenges include:[10][5]
- Routine maintenance and cleaning needs to be done regularly
- Routine maintenance as well as major overhauls and capital replacement need to be planned and budgeted for in advance
- Lack of funding for spare parts
- Lack of local qualified technicians
- Emergency back-up generators should be checked periodically even if rarely used
- Improper or insufficient maintenance can lead to substantial costs in the future
Regular maintenance is well worth the cost, and programs installing energy systems at health clinics or other facilities should ensure there will be a commitment to servicing the system. Experts recommend training local personnel in the servicing of these systems or obtaining a long-term maintenance contract with a service provider.
Financing of Operation and Maintenance
Financing of renewable energy system use and maintenance, including component replacements, is key to system sustainability in the long run. Oftentimes the most difficult question to resolve is how to pay for component replacements, from light bulbs to batteries.[11] A lack of funding for operating and maintenance can result in unusable equipment.
Clinic managers must develop a sustainable way to pay for the maintenance and operation of the system to ensure continuity of facility operations. Facilities could consider incorporating aspects of the finance structures described below by USAID into their financial and operating practices.[5]
User Fees
A “user fee” system involves building the cost of energy into the overall cost of medical services – passing the cost to the patient. Most rural healthcare facilities struggle to secure sufficient operating funds due to the inability to pass along true costs of medical service to users who lack the resources to pay actual costs. The inability of patients to pay, coupled with the challenge of managing the collection and disbursement of funds, makes this approach difficult to implement.[5]
Sale of Excess Electricity
The sale of excess electricity offers a promising approach to finance operations. By installing a mini-grid system with excess capacity, income from the sale of additional electricity can offset a portion, if not all, of the system’s operating costs.
- Bulk (Wholesale): By operating the power system as a small enterprise, excess electricity can be sold to nearby villages, factories, schools or facilities. The system must be sized to accommodate both the clinic and the potential customer base. Customers must be in close proximity to the system or transmission costs quickly make this approach prohibitively expensive. Maintenance requirements are also more complex, thus budgets to be planned in need to be higher.[5] Insufficient interaction between medical, building and engineering staff, and utilities can be another barrier for leveraging the electricity generation potential of health facilities for broader community needs. Careful planning and capacity building is necessary.[2][12]
- Point of Use Sale (Retail): When potential purchasers of power are too remote to obtain the electricity over transmission lines, the clinic can sell it at or near their facility. A small powering station can be established with fees charged based on the amount of power used, if metering is available, or according to time. For customers with transportable devices such as power tools, a small work area with outlets can be set aside adjacent to the power station where users can plug in equipment. Villagers can use these areas for income-generating activities. It may be feasible to establish a “mini industrial zone” near the clinic’s power system, providing an area with permanent workshops (sewing, weaving or repair services) or stores. The clinic could realize income from rent on the workshop/store space, the sale of electricity, and the pumping of water.[5]
Productive Uses within the health center premises
Using the excess electricity for productive uses like running a canteen/restaurant, offering phone charging, sale of cold drinks/food requiring refrigerations within the health center premises can serve as a potential source of income for O&M of the solar systems. GIZ Uganda is piloting this model in health centers in displacement settings in Uganda in 2021/2022. [13]
Institutional Management
As the finance provider, the system installer, and system owner are almost always different actors, clear arrangements are needed regarding a division of responsibilities, ownership and accountability to keep the energy system functioning. Lacking ownership or capability of institutions can be encountered by careful planning, stakeholder engagement, sensitization, and capacity building to achieve organizational sustainability.[8] Having an entity that has a stake in the continued successful operation of the system is crucial to cultivating a sense of ownership for ongoing system operation.
Stepwise Approach to Electrifying a Health Center
According to USAID:[5]
- Identify the Health Center's Current Energy Demands
Identify current energy needs and applications, e.g. for lighting, refrigeration, communication, etc. - Account for Near-Term Change
Determine whether energy demands will change in the near-term. - Establish Target Energy Consumption in kWh/day
Use tools such as the USAID Health Clinic Power System Design Tool (4 - Electric Load Inputs) or the Energy Audit Spreadsheet (Worksheet 7 - Future Electric Applications) to calculate the future electric energy consumption in kWh/day. - Determine Technologies Needed to Meet Target
Evaluate energy technologies. - Procure, Design System, and Install Technology
Select the most appropriate energy technology. - Maintain and Financing Your Energy Technology
Institute financing mechanism(s) accounting for operation and maintenance needs and costs.
Remember to contact an expert for assessment, system design, procurement, installation, and maintenance of energy technologies!
Thermal Energy for Health Facilities
In addition to electricity, health facilities need thermal energy for food preparation, water and space heating, sterilization of equipment and medical waste incineration. Also for cooling in applications such as absorption refrigeration (using LPG or kerosene), thermal energy may be used.
In general, there is little focus and information on thermal energy demand and supply of health facilities to be found in literature and studies.
In settings, where access to electricity is no problem, some or all thermal needs may be met with electric-powered appliances. However, very often the reality of rural health centers is different: thermal energy is mainly produced through direct combustion of fuel, e.g. firewood or charcoal, gas, kerosene or diesel.[2]
Food Preparation
In most rural health facilities, thermal energy is needed for food preparation – for staff as well as for patients.
Food for Staff
It depends mainly on the number of staff, the health center management and/or the degree of self-organization of the staff if the meals for staff members are prepared communally. In this case an institutional size stove might make sense.
Examples: Both Mission and the Government hospitals in Mulanje District (Southern Malawi) have institutional size wood-fired rocket stoves to cater for the staff and the students of the nursing college. Cooking is done by a paid cook, who got trained by GIZ on the proper use of the stoves. The firewood is provided by the hospital. Savings as compared to the open fire are between 70-80 percent.
Food for Patients
Most rural health centers do not provide meals for the patients, even if they have in-patient facilities. Usually, the meals for patients are prepared individually by the guardians who accompany the patient often with the main purpose to cater or prepare warm bath water for the patient. Thus individual cooking facilities are needed for the guardians. Usually food ingredients, fuel and cooking utensils have to be organized by the guardians and are not provided by the health center. Thus the most prevalent cooking facility is the 3-stone fire fueled with firewood or any other biomass that the guardians are able to organize in the immediate surroundings of the health center. A good practice is when health centers provide a sheltered cooking place and define the area where cooking is allowed. To minimize the adverse effects of air pollution and prevent that smoke is adding to the ailments of the patients, this location should preferably be at a distance from the wards and care units.
Mulanje Mission Hospital in Southern Malawi went even further: they had already a roofed kitchen for the guardians with 20 simple fireplaces. As hospital facilities were expanding and the number of in-patients increasing, the kitchen became too small. With advice from GIZ-project staff on stove technology and kitchen design, they added another roofed kitchen with improved fixed ‘Esperanza’ -type stoves and good ventilation. In the first weeks the kitchen was not yet well accepted and rather empty, because people were not familiar with the stoves and were unsure how to use them. Upon realizing this, a permanent security staff of the hospital got trained on the correct stove use and was able to show the ever-changing users, who normally don’t use the kitchen longer than a few days. From then onward the kitchen became more and more popular as people became aware of the advantages: the new stoves were more economic, cooked faster, created less smoke, and the building had a better ventilation. Young mothers felt more comfortable bringing their babies in the new kitchen. The challenge is to organize the maintenance of the stoves, as some of the ceramic pot-supports of the ‘Esperanza stoves’ had gone missing and the stoves performed poorly without them.
Sterilization / Pasteurization / Water Heating
Thermal energy is also needed for the sterilization of instruments, the pasteurization of drinking water and to heat bath water for the patients. Thermo-solar energy might be an option, if used with a (reusable) temperature indicator to ensure that the water has reached the required temperature. Solar energy is also a good option to heat bath water for the patients, if storage of hot water is provided. Conventional passive solar thermal water heating systems are becoming more common in developing countries, and can usually heat water to a temperature suitable for basic hygiene and sanitation.[2]
Space Heating
Space heating is important in health facilities in temperate climates, and during the cold season of higher-altitude zones of Central Asia, Latin America and Africa, as well as the Mediterranean.
Space heating in developing-country health facilities may be provided by district heating, electricity or on-site fuel-based solutions. Inexpensive thermal solar panels can also provide hot water for space heating.
Improving the energy efficiency of buildings can greatly reduce thermal energy needs as well as electricity requirements.[2]
Project Experience
- Experience and lessons learned, including project approaches, technical details and evidence for impacts of GIZ projects in Uganda and Ethiopia are discussed in the article "Photovoltaic (PV) for Health Centers - Project Experience". It aims at compiling experience from past and ongoing PV programmes for rural health centers.
- Sustainable energy access for social institutions through service models
According to surveys conducted by the Green People’s Energy (GBE, Grüne Bürgerenergie) Benin project between 2020–2021, more than 69% of the solar systems installed up to five years prior by various electrification efforts (donors, government, charities) in health centers were no longer functioning. In order to ensure the sustainability of solar systems installed for the benefit of social institutions, the German cooperation-financed GBE Programme implemented by GIZ, pilots service-based delivery models in Benin that are based on a long-term commitment of a service provider (i.e. a solar company) to maintain the system and of the client (i.e. the social institution) to pay a monthly fee.
Read more about this approach here.
- Improving Health Services for the Rural Population in Ghana
A project by the Green People’s Energy (Grüne Bürgerenergie, GBE) aims at improving the conditions for rural communities to use renewable energy applications in their social infrastructure by supporting 31 clinics. The clinics were selected by the Ghana Health Service, the state-owned agency responsible for the operation and maintenance of around 500 rural clinics in Ghana, jointly with the Ministry of Energy and GBE.
Read more about the project and its lessons learned here.
- Improved Energy Access for the Kaffrine Region
Kaffrine is a rural region in Senegal where more than half of the population and social institutions (e.g. schools and health posts) do not have access to electricity from the national grid. The GBE project supports the acquisition, sustainable management, and financial viability of solar systems for the benefit of ten rural sewing craft enterprises, eight schools and five health centres in Kaffrine.
Read more about the project here.
Further Information
- Webinar on Powering Humanitarian Health Operations: Sustainable Energy Solutions
- Articles on energypedia:
- SEforAll, The World Bank (2021): Powering Healthcare Solutions Catalogue.
- Powering Health, USAID website covering all major issues on electricity supply for rural health centers. Several country case studies available. Offers tools for energy audits and load calculation. Highly recommandable!
- USAID: Powering Health: Electrification Options for Rural Health Centers - Step-by-step guide on energy needs, power generation options, and sustainability issues for rural health centers. Case studies from Botswana and Uganda.
- ESMAP (2010): Photovoltaics for Community Service Facilities". This very resourceful handbook covers the most relevant issues regarding sustainability and long-term operation of community PV systems.
- Practical Action (2007): Solar PV Refrigeration of Vaccines - Technical Background of solar refrigeration
- IEA (2014): PV Systems for Rural Health Facilities in Developing Areas.pdf
- National Renewable Energy Laboratory USA (1998): Renewable Energy for Rural Health Clinics- Publication on energy issues of rural health clinics: energy applications, electrical system components, system selection and economics, institutional considerations. Also provides case studies and lessons learned.
- The World Bank (2020): Increasing Human Capital by Electrifying Health Centers and Schools through Off-Grid Solar Solutions. Live Wire Brief 2020/104
- IRENA, UNSD, World Bank, WHO. 2020. Tracking SDG 7: The Energy Progress Report. Chapter 1 Access to Electricity.
References
- ↑ India Today (2019). https://www.indiatoday.in/india/story/after-4-years-of-swachh-bharat-38-percent-govt-health-centres-in-rural-india-without-staff-toilets-1623694-2019-12-04
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 WHO, The World Bank (2015): Access to modern energy services for health facilities in resource-constrained settings: a review of status, significance, challenges and measurement.
- ↑ UN Foundation, SEforALL (2019): Lasting impact – Sustainable off-grid solar delivery models to power health and education. https://poweringhc.org/wp-content/uploads/2019/04/Lasting-Impact_Sustainable-Off-Grid-Solar-Delivery-Models-to-Power-Health-and-Education.pdf
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 IEA PVPS Task 9 (2014): PV Systems for Rural Health Facilities in Developing Areas. https://energypedia.info/images/b/bf/PV_Systems_for_Rural_Health_Facilities_in_Developing_Areas.pdf
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 USAID (no date): Powering Health: Electrification Options for Rural Health Centers. http://pdf.usaid.gov/pdf_docs/PNADJ557.pdf
- ↑ 6.0 6.1 Smart Villages (2017): Electrification of health clinics in rural areas: Challenges and opportunities. https://e4sv.org/wp-content/uploads/2017/05/TR12-Electrification-of-health-clinics-in-rural-areas-Challenges-and-opportunities_web.pdf
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Franco et al./Sustainable Energy Technologies and Assessments 22 (2017) 92–105. A review of sustainable energy access and technologies for healthcare facilities in the Global South. https://www.sciencedirect.com/science/article/pii/S2213138817301376?via%3Dihub
- ↑ 8.0 8.1 UN Foundation, SEforALL (2019): Lasting impact – Sustainable off-grid solar delivery models to power health and education. http://poweringhc.org/wp-content/uploads/2019/04/Lasting-Impact_Sustainable-Off-Grid-Solar-Delivery-Models-to-Power-Health-and-Education.pdf
- ↑ https://en.wikipedia.org/wiki/Micro_hydro
- ↑ 10.0 10.1 World Bank (2017): State of Electricity Access Report, Special Feature - Modern Energy Access and Health. http://documents.worldbank.org/curated/en/756131494939083421/pdf/BRI-P148200-PUBLIC-FINALSEARSFHealthweb.pdf
- ↑ ESMAP 2010: Photovoltaics for Community Service Facilities http://documents.worldbank.org/curated/en/837791468332067596/pdf/632250WP0Photo00Box0361508B0PUBLIC0.pdf
- ↑ WHO, The World Bank (2015): Access to modern energy services for health facilities in resource-constrained settings: a review of status, significance, challenges and measurement. https://apps.who.int/iris/bitstream/handle/10665/156847/9789241507646_eng.pdf%3Bjsessionid=05BA6EDD62617D7CFB7AE8FBE47A639A?sequence=1
- ↑ Electrification of Health Centers in Displacement Settings: https://energypedia.info/images/8/8a/Electrification_of_Health_Centers_in_Displacement_Setting.pdf Webinar Series on Decarbonisation of Energy Infrastructure in Displacement Situations